Overview
Hypertension; Hypertension (HTN), defined as systolic blood pressure (SBP) > 140 mmHg or diastolic blood pressure (DBP) > 90 mmHg, affects around 40 % of the worldwide population aged over 25 years, and is estimated to be implicated in approximately half of the deaths from stroke or cardiovascular disease, an estimated 970 million people worldwide suffer from the disease resulting in significant morbidity, mortality and financial burden globally. Diagnosing and treating hypertension plays an important role in minimising the risk of cardiovascular disease and stroke. Early and accurate diagnosis of hypertension, as well as regular monitoring, is essential to meet treatment targets. It is estimated that uncontrolled HTN is responsible for 7.5 million deaths per year worldwide and in USA alone 75 million people affect from hypertension, and accounts for over 47 billion dollars spent in health care services, medications and absent workforce.
Based on recommendations of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7), the classification of BP for adults aged 18 years or older has been as follows:
- Normal: Systolic lower than 120 mm Hg, diastolic lower than 80 mm Hg
- Prehypertension: Systolic 120-139 mm Hg, diastolic 80-89 mm Hg
- Stage 1: Systolic 140-159 mm Hg, diastolic 90-99 mm Hg
- Stage 2: Systolic 160 mm Hg or greater, diastolic 100 mm Hg or greater
Hypertension may be primary, which may develop as a result of environmental or genetic causes, or secondary, which has multiple etiologies, including renal, vascular, and endocrine causes. Primary or essential hypertension accounts for 90-95% of adult cases, and secondary hypertension accounts for 2-10% of cases.
It happens when the force of the blood pumping through your arteries is too strong. When your heart beats, it pushes blood through your arteries to the rest of your body. When the blood pushes harder against the walls of your arteries, your blood pressure goes up. Your blood pressure may be different at different times of the day. It is usually higher when you first wake up, after you exercise, or when you are under stress.
Measuring Blood Pressure
How is Blood Pressure Measured?Usually, a cuff is filled with air to squeeze the artery in your upper arm while a “gauge” (measuring tool) records your blood pressure as the air is released from the cuff. Most home devices use digital (electronic) gauges.

What Do the Numbers Mean?
A blood pressure measurement has two parts—a top (first) number and a bottom (second) number. The top number is the “systolic” (pronounced sis-TOL-ik) pressure and the bottom number is the “diastolic” (pronounced di-a-STOL-ik) pressure.
- Systolic pressure is your blood pressure when your heart beats and pumps blood through your arteries. Your blood pressure is higher while your heart is pumping, so the systolic number is higher.
- Diastolic pressure is your blood pressure in between heartbeats when your heart is not pumping. Your blood pressure is lower while your heart is not pumping, so the diastolic number is lower.
Your blood pressure numbers are given one on top of the other, with your systolic pressure “over” your diastolic pressure.
- A normal blood pressure is less than “120 over 80,” or 120/80. This means the systolic pressure is 120 and the diastolic pressure is 80.
- A blood pressure between 120/80 and 139/89 is called “prehypertension.” This means that your blood pressure is higher than normal and that you are at risk for having high blood pressure.
- If your blood pressure is 140/90 or higher most of the time it is measured, you have high blood pressure.
Symptoms of High Blood Pressure
Most people with high blood pressure have no signs or symptoms, even if blood pressure readings reach dangerously high levels. It may take years or even decades for the condition to reach levels severe enough that symptoms become obvious. Even then, these symptoms may be attributed to other issues.
Symptoms of hypertension include:
- headaches
- shortness of breath
- nosebleeds
- flushing
- dizziness
- chest pain
- visual changes
- blood in the urine
These symptoms don’t occur in everyone with hypertension, but waiting for a symptom of this condition to appear could be fatal. The best way to know if you have hypertension is to get regular blood pressure readings. Most doctors’ offices will take a blood pressure reading at every appointment.
Causes of Hypertension
There are two types of hypertension. Each type has a different cause.
Primary hypertension
Primary hypertension is also called essential hypertension. This kind of hypertension develops over time with no identifiable cause. Researchers are still unclear what mechanisms cause blood pressure to slowly increase. A combination of factors may play a role. These factors include:
- Genes: Some people are genetically predisposed to hypertension. This may be from gene mutations or genetic abnormalities inherited from your parents.
- Physical changes: If something in your body malfunctions, you may begin experiencing issues throughout your body. High blood pressure may be one of those issues.
- Environment: Over time, unhealthy lifestyle choices like lack of physical activity and poor diet can take their toll on your body. Lifestyle choices can lead to weight problems. Being overweight or obese can increase your risk for hypertension.
For example, it’s thought that changes in your kidney function may upset the body’s natural balance of salts and fluid. This change may cause your body’s blood pressure to increase.
Although the aetiology of essential HTN is unknown, it is often associated with increased salt intake and obesity and has a strong relationship with family history, underscoring the possibility of genetic predisposition for the disease
Secondary hypertension
Secondary hypertension often occurs quickly and can become more severe than primary hypertension. Several conditions that may cause secondary hypertension include:
- chronic kidney disease
- congenital heart defects
- problems with your thyroid
- side effects of medications
- use of illegal drugs
- alcohol abuse or chronic use
- adrenal gland problems
- certain endocrine tumors
- sleep apnea
- renal artery stenosis
The common phenomenon in both scenarios is the derangement of multiple mechanisms involved in the maintenance of normal blood pressures and as such, the sympathetic nervous system, renin-angiotensin-aldosterone system, endothelial function plus sodium and water retention have been extensively studied to ascertain mechanisms involved in the development of the disease.
Cardiac output and peripheral vascular resistance (PVR)
Cardiac output and PVR are two important factors that maintain normal blood pressures and it has been suggested that increased cardiac output resulting from sympathetic dysfunction is the trigger for the development of HTN and increases in PVR is essentially the physiologic response to accommodate change in pressure and maintain homeostasis.
Sympathetic nervous system
Over the last decade the role of SNS in the development and maintenance of blood pressure has been studied exhaustively and it has been identified that sympathetic stimulation of the heart, peripheral vasculature, and kidneys, resulting in increased cardiac output, increased vascular resistance, plus fluid retention is important in the development and maintenance of this disease. As evidenced in the Coronary Artery Risk Development in Young Adults (CARDIA) study, sympathetic overdrive is often accompanied by low parasympathetic tone, which further exacerbates the condition. The renal sympathetic nervous system is a major player in the development and maintenance of HTN affecting blood pressure via two pathways, namely, the efferent and afferent pathways. The efferent pathway carries signals from the SNS to the kidney and increases renin release thereby activating the RAAS system and increasing sodium and water retention, all resulting in increased circulating volumes and therefore increased blood pressures. In addition to the aforementioned processes the efferent pathway also decreases renal blood flow and to increase perfusion the kidney triggers the afferent pathway that carries impulses to the SNS exacerbating sympathetic over activity and thereby maintaining the high blood pressures.
Renin-angiotensin-aldosterone system (RAAS)
The RAAS system plays a major role in orchestrating the maintenance of normal blood pressures and is activated by dual mechanisms, stimulation of the SNS and glomerular under perfusion. These stimuli trigger the release of renin from the juxtaglomerular apparatus which converts angiotensinogen to inactive angiotensin I, the latter is further cleaved by endothelium bound angiotensin converting enzyme (ACE) into angiotensin II, the active component of this cascade and a potent vasoconstrictor. Although this conversion of angiotensin I to angiotensin II was initially believed to occur primarily in the lungs, it has since been established that the process occurs practically in all tissues. In response to decreased salt intake RAAS also triggers the release of aldosterone from the adrenal glands that increases salt reabsorption coupled with water retention resulting in further increase of blood pressure. Under these circumstances one would expect that patients with HTN would invariably have high circulating levels of renin and angiotensin II, however, studies have demonstrated that plasma renin activity is increased in 15 percent patients, normal in 60 percent patients, and reduced in approximately 25 percent patients. This can be reconciled by growing evidence for the presence of local renin systems regulating regional blood flow that might play an essential part in the pathophysiology of HTN.
Endothelial dysfunction
Whether endothelial dysfunction is a cause or an effect of hypertension is debatable, nonetheless there is substantial evidence linking endothelial dysfunction with hypertension. In fact, there is evidence of a positive association between the degree of endothelial dysfunction and the severity of hypertension. The major underlying mechanism for endothelial dysfunction seen in HTN is the decrease in the availability of nitric oxide (NO), a consequence of increased oxidative stress in these patients. To this, extent although effective antihypertensive therapy restores impaired nitric oxide production, endothelium dependent vasorelaxation continues to be altered suggesting an irreversible course once HTN is established. This evidence as well as studies demonstrating that inhibition of endothelium-derived nitric oxide synthase (eNOS) results in hypertension in humans, insinuates endothelial dysfunction as a potential aetiological factor in the initiation of HTN. On the other hand the Multiethnic Study of Atherosclerosis (MESA) showed that impaired flow-mediated dilation (FMD) was not a significant independent predictor of the future development of hypertension and an association of higher blood pressures in adolescence with endothelial dysfunction in adulthood. In addition to NO other vasorelaxing factors such as arachidonic acid metabolites, reactive oxygen species (ROS), vasoactive peptides and microparticles of endothelial origin play important roles in maintenance of vascular tone. Emerging data suggests that these factors contribute to excessive vascular oxidative stress and vascular inflammation resulting in endothelial dysfunction. In the recent years endothelial progenitor cells (EPC’s) that develop to form mature endothelial cells has been implicated in the maintenance of arterial stiffness and as such are now considered as determinants of endothelial function. Thus endothelial dysfunction is multifactorial and a myriad of alterations in the vascular milieu lead to structural and functional changes within the arteries and therapies targeting key pathways involved in the process have shown to decrease vascular remodeling, improve vascular function and therefore attenuate overall cardiovascular risk.
Whilst due to its relevance endothelial function was initially measured in the coronary arteries invasively using acetylcholine or other pharmacologic flow manipulation, current methodologies include venous plethysmography, digital pulse tonometery, laser Doppler flowmetry and the most common high-resolution ultrasound. These methods have not only made early identification of endothelial dysfunction possible and but has also broadened the horizon of FMD in determining efficacy of treatment and assessing prognosis in patients with HTN and other cardiovascular diseases.
Vasoactive substances
Endothelin, a potent vasoconstrictor is one of the major substances involved in maintaining vascular tone. It is secreted by endothelial cells and exerts its affects in a paracrine or autocrine manner on vascular smooth muscle cells and counteracts the relaxing activity of NO Studies have demonstrated that both in animals and humans infusion of endothelin-1 (ET-1) results in increased blood pressures and blocking the system using antagonists reverts the phenomenon [49]. However, plasma levels of ET-1 are normal in patients with essential hypertension suggesting that activity of this system might not play a role in all types of HTN but rather in specific disease states such as salt-sensitive HTN and renal HTN. Large clinical trials aimed at determining both the importance of endothelin in the development and maintenance of HTN and, ascertaining necessity of treatments targeted towards maintenance of this system are warranted.
Bradykinin a vasodilatory peptide with autocrine and paracrine function has long had an indirect association with HTN since apart from its direct vasodilatory affects, bradykinin stimulates release of other vasoactive substances like prostaglandins. This peptide from the kinin-kallikrein system is shown to reduce blood pressures by vasodilation as well as enhanced natriuresis and diuresis both achieved via increased renal blood flow mediated by NO and prostaglandin release. Although vastly overlooked due to side effects of coughing and angioedema the hypotensive effects of ACE inhibitors is due to increased bradykinin levels owing to its reduced degradation therefore therapies targeted directly at bradykinin system are likely in the not so distant future.
Atrial natriuretic peptide (ANP) belongs to a family of structurally and functionally related peptide hormones with cardio-renal functions. ANP mediates its functions via membrane-bound guanylatecyclase linked receptor (NPR-A), which further activates intracellular cGMP mediated processes. Released from the atria in response to atrial distention stemming from hemodynamic overload, ANP causes natriuresis and diuresis resulting in modest reductions in blood pressures with concomitant decreases in plasma renin and aldosterone. Thus, the natriuretic peptide system by decreasing peripheral vascular resistance balances the activity of the SNS and the RAAS system in maintaining blood pressures.
Risk factors
High blood pressure has many risk factors, including:
- Age: The risk of high blood pressure increases as you age. Through early middle age, or about age 45, high blood pressure is more common in men. Women are more likely to develop high blood pressure after age 65.
- Race: High blood pressure is particularly common among blacks, often developing at an earlier age than it does in whites. Serious complications, such as stroke, heart attack and kidney failure, also are more common in blacks.
- Family history: High blood pressure tends to run in families.
- Being overweight or obese: The more you weigh the more blood you need to supply oxygen and nutrients to your tissues. As the volume of blood circulated through your blood vessels increases, so does the pressure on your artery walls.
- Not being physically active: People who are inactive tend to have higher heart rates. The higher your heart rate, the harder your heart must work with each contraction and the stronger the force on your arteries. Lack of physical activity also increases the risk of being overweight.
- Using tobacco: Not only does smoking or chewing tobacco immediately raise your blood pressure temporarily, but the chemicals in tobacco can damage the lining of your artery walls. This can cause your arteries to narrow, increasing your blood pressure. Secondhand smoke also can increase your blood pressure.
- Too much salt (sodium) in your diet: Too much sodium in your diet can cause your body to retain fluid, which increases blood pressure.
- Too little potassium in your diet: Potassium helps balance the amount of sodium in your cells. If you don’t get enough potassium in your diet or retain enough potassium, you may accumulate too much sodium in your blood.
- Too little vitamin D in your diet: It’s uncertain if having too little vitamin D in your diet can lead to high blood pressure. Vitamin D may affect an enzyme produced by your kidneys that affects your blood pressure.
- Drinking too much alcohol: Over time, heavy drinking can damage your heart. Having more than two drinks a day for men and more than one drink a day for women may affect your blood pressure.If you drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women of all ages and men older than age 65, and up to two drinks a day for men age 65 and younger. One drink equals 12 ounces of beer, 5 ounces of wine or 1.5 ounces of 80-proof liquor.
- Stress: High levels of stress can lead to a temporary increase in blood pressure. If you try to relax by eating more, using tobacco or drinking alcohol, you may only increase problems with high blood pressure.
- Certain chronic conditions: Certain chronic conditions also may increase your risk of high blood pressure, such as kidney disease, diabetes and sleep apnea.
Sometimes pregnancy contributes to high blood pressure, as well.
Although high blood pressure is most common in adults, children may be at risk, too. For some children, high blood pressure is caused by problems with the kidneys or heart. But for a growing number of kids, poor lifestyle habits, such as an unhealthy diet, obesity and lack of exercise, contribute to high blood pressure.
Diagnosis of Hypertension
Measurement of blood pressures can be done either manually using a sphygmomanometer or an automated electronic device (both office and home) or when feasible ambulatory blood pressure monitoring is utilized. The latter two are preferred since they are reproducible and rule out observer bias. Readings are measured in both arms using arm cuffs for accuracy. The use of finger cuffs is strongly discouraged due to lack of reproducibility. Blood pressure measurements are taken on an empty bladder with the patient well positioned, legs resting on the ground and arms resting comfortably on a table. An average of two readings taken approximately 5 minutes apart is taken at two visits to determine blood pressure. In older patients postural hypertension is also assessed. In addition to blood work and electrocardiography, it is important to consider all previous cardiovascular events, risk factors plus other medical and medication history (stroke, transient ischemic attacks, coronary artery disease, heart failure, chronic kidney disease, peripheral artery disease, diabetes and sleep apnea) to determine an appropriate treatment plan.
If your blood pressure remains high, your doctor will likely conduct more tests to rule out underlying conditions. These tests include:
- urine test
- cholesterol screening
- test of your heart’s electrical activity
These tests can help your doctor identify any secondary issues causing your elevated blood pressure.
Treatment of High Blood Pressure
Non-Pharmacological Options
The recommendations to lower BP and decrease cardiovascular disease risk include the following, with greater results achieved when 2 or more lifestyle modifications are combined:
- Weight loss (range of approximate systolic BP reduction [SBP], 5-20 mm Hg per 10 kg)
- Limit alcohol intake to no more than 1 oz (30 mL) of ethanol per day for men or 0.5 oz (15 mL) of ethanol per day for women and people of lighter weight (range of approximate SBP reduction, 2-4 mm Hg)
- Reduce sodium intake to no more than 100 mmol/day (2.4 g sodium or 6 g sodium chloride; range of approximate SBP reduction, 2-8 mm Hg)
- Maintain adequate intake of dietary potassium (approximately 90 mmol/day)
- Maintain adequate intake of dietary calcium and magnesium for general health
- Stop smoking and reduce intake of dietary saturated fat and cholesterol for overall cardiovascular health
- Engage in aerobic exercise at least 30 minutes daily for most days (range of approximate SBP reduction, 4-9 mm Hg)
Although diet and exercise are the most appropriate tactics to lower your blood pressure, some supplements also may help lower it. However, more research is needed to determine the potential benefits. These include:
- Fiber, such as blond psyllium and wheat bran
- Minerals, such as magnesium, calcium and potassium
- Folic acid
- Supplements or products that increase nitric oxide or widen blood vessels (vasodilators), such as cocoa, coenzyme Q10, L-arginine or garlic
- Omega-3 fatty acids, found in fatty fish, fish oil supplements or flaxseed
Pharmacological Treatments
- Thiazide diuretics. Diuretics, sometimes called water pills, are medications that act on your kidneys to help your body eliminate sodium and water, reducing blood volume. Thiazide diuretics are often the first, but not the only, choice in high blood pressure medications. Thiazide diuretics include hydrochlorothiazide (Microzide), chlorthalidone and others.If you’re not taking a diuretic and your blood pressure remains high, talk to your doctor about adding one or replacing a drug you currently take with a diuretic. Diuretics or calcium channel blockers may work better for black and older people than do angiotensin-converting enzyme (ACE) inhibitors alone. A common side effect of diuretics is increased urination.
- Beta blockers. These medications reduce the workload on your heart and open your blood vessels, causing your heart to beat slower and with less force. Beta blockers include acebutolol (Sectral), atenolol (Tenormin) and others.When prescribed alone, beta blockers don’t work as well, especially in black and older people, but may be effective when combined with other blood pressure medications.
- Angiotensin-converting enzyme (ACE) inhibitors. These medications — such as lisinopril (Zestril), benazepril (Lotensin), captopril (Capoten) and others — help relax blood vessels by blocking the formation of a natural chemical that narrows blood vessels. People with chronic kidney disease may benefit from having an ACE inhibitor as one of their medications.
- Angiotensin II receptor blockers (ARBs). These medications help relax blood vessels by blocking the action, not the formation, of a natural chemical that narrows blood vessels. ARBs include candesartan (Atacand), losartan (Cozaar) and others. People with chronic kidney disease may benefit from having an ARB as one of their medications.
- Calcium channel blockers. These medications — including amlodipine (Norvasc), diltiazem (Cardizem, Tiazac, others) and others — help relax the muscles of your blood vessels. Some slow your heart rate. Calcium channel blockers may work better for black and older people than do ACE inhibitors alone.Grapefruit juice interacts with some calcium channel blockers, increasing blood levels of the medication and putting you at higher risk of side effects. Talk to your doctor or pharmacist if you’re concerned about interactions.
- Renin inhibitors. Aliskiren (Tekturna) slows down the production of renin, an enzyme produced by your kidneys that starts a chain of chemical steps that increases blood pressure.Tekturna works by reducing the ability of renin to begin this process. Due to a risk of serious complications, including stroke, you shouldn’t take aliskiren with ACE inhibitors or ARBs.
Additional Medications Sometimes Used to Treat High Blood Pressure
If you’re having trouble reaching your blood pressure goal with combinations of the above medications, your doctor may prescribe:
- Alpha blockers. These medications reduce nerve impulses to blood vessels, reducing the effects of natural chemicals that narrow blood vessels. Alpha blockers include doxazosin (Cardura), prazosin (Minipress) and others.
- Alpha-beta blockers. In addition to reducing nerve impulses to blood vessels, alpha-beta blockers slow the heartbeat to reduce the amount of blood that must be pumped through the vessels. Alpha-beta blockers include carvedilol (Coreg) and labetalol (Trandate).
- Central-acting agents. These medications prevent your brain from signaling your nervous system to increase your heart rate and narrow your blood vessels. Examples include clonidine (Catapres, Kapvay), guanfacine (Intuniv, Tenex) and methyldopa.
- Vasodilators. These medications, including hydralazine and minoxidil, work directly on the muscles in the walls of your arteries, preventing the muscles from tightening and your arteries from narrowing.
- Aldosterone antagonists. Examples are spironolactone (Aldactone) and eplerenone (Inspra). These drugs block the effect of a natural chemical that can lead to salt and fluid retention, which can contribute to high blood pressure.
To reduce the number of daily medication doses you need, your doctor may prescribe a combination of low-dose medications rather than larger doses of one single drug. In fact, two or more blood pressure drugs often are more effective than one. Sometimes finding the most effective medication or combination of drugs is a matter of trial and error.
Complications
The excessive pressure on your artery walls caused by high blood pressure can damage your blood vessels, as well as organs in your body. The higher your blood pressure and the longer it goes uncontrolled, the greater the damage.
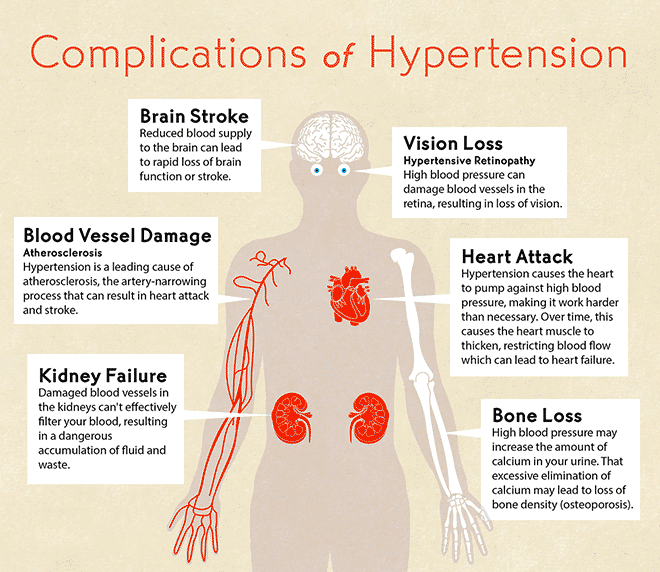
Uncontrolled high blood pressure can lead to:
- Heart attack or stroke. High blood pressure can cause hardening and thickening of the arteries (atherosclerosis), which can lead to a heart attack, stroke or other complications.
- Aneurysm. Increased blood pressure can cause your blood vessels to weaken and bulge, forming an aneurysm. If an aneurysm ruptures, it can be life-threatening.
- Heart failure. To pump blood against the higher pressure in your vessels, your heart muscle thickens. Eventually, the thickened muscle may have a hard time pumping enough blood to meet your body’s needs, which can lead to heart failure.
- Weakened and narrowed blood vessels in your kidneys. This can prevent these organs from functioning normally.
- Thickened, narrowed or torn blood vessels in the eyes. This can result in vision loss.
- Metabolic syndrome. This syndrome is a cluster of disorders of your body’s metabolism, including increased waist circumference; high triglycerides; low high-density lipoprotein (HDL) cholesterol, the “good” cholesterol; high blood pressure; and high insulin levels. These conditions make you more likely to develop diabetes, heart disease and stroke.
- Trouble with memory or understanding. Uncontrolled high blood pressure may also affect your ability to think, remember and learn. Trouble with memory or understanding concepts is more common in people with high blood pressure.